Examinations Under Anaesthesia
THE GOOD, THE BAD & THE UGLY
What exactly is a Examination Under Anaesthesia?
This is a surgical examination under general or spinal anaesthesia, also known as a EUA. Due to the location of a particular area that requires a deeper look, a surgeon will usually advocate for this procedure to minimise pain and discomfort to the patient.
Why you might have one and the benefits
This procedure can be performed in order to establish a diagnosis in patients with pain around the back passage that cannot be examined in a clinic or as part of a procedure. They happen most frequently if you require investigations for cancer of the rectum or cervix. But they are also used in other areas of surgery to relieve symptoms of fistulas, haemorrhoids and fissures.
As you are either asleep under general or giving a spinal anaesthetic, the procedure is free of pain and discomfort. It is also very quick, probably a maximum of 40 minutes, depending on what is being investigated, which you’ll be made aware of before the procedure.
Recovery is the same day, as most will be done as day surgery cases. Being allowed home can occur once you are eating and drinking, are able to manage the pain and walk unaided and have passed some urine.
Biopsies can be taken during the procedure, or setons and drains can be left in situ as part of a treatment plan discussed with you when consenting to the procedure. Follow up for those will be discussed on discharged and booked for you.
Use in IBD
In IBD, examinations under anaesthesia are commonly used most in patients who have perianal Crohn’s disease. In this type of IBD, the inflammatory response of the disease is located to the perineum which can possibly involve fistulas, abscesses and fissures. Due to the location of these issues occurring, they can take a while to heal and may require further, more long term treatment with more EUAs being planned in.
They can also be used when the healing of wounds – such as proctectomy wounds – is not complete and abscesses develop.
My Experience
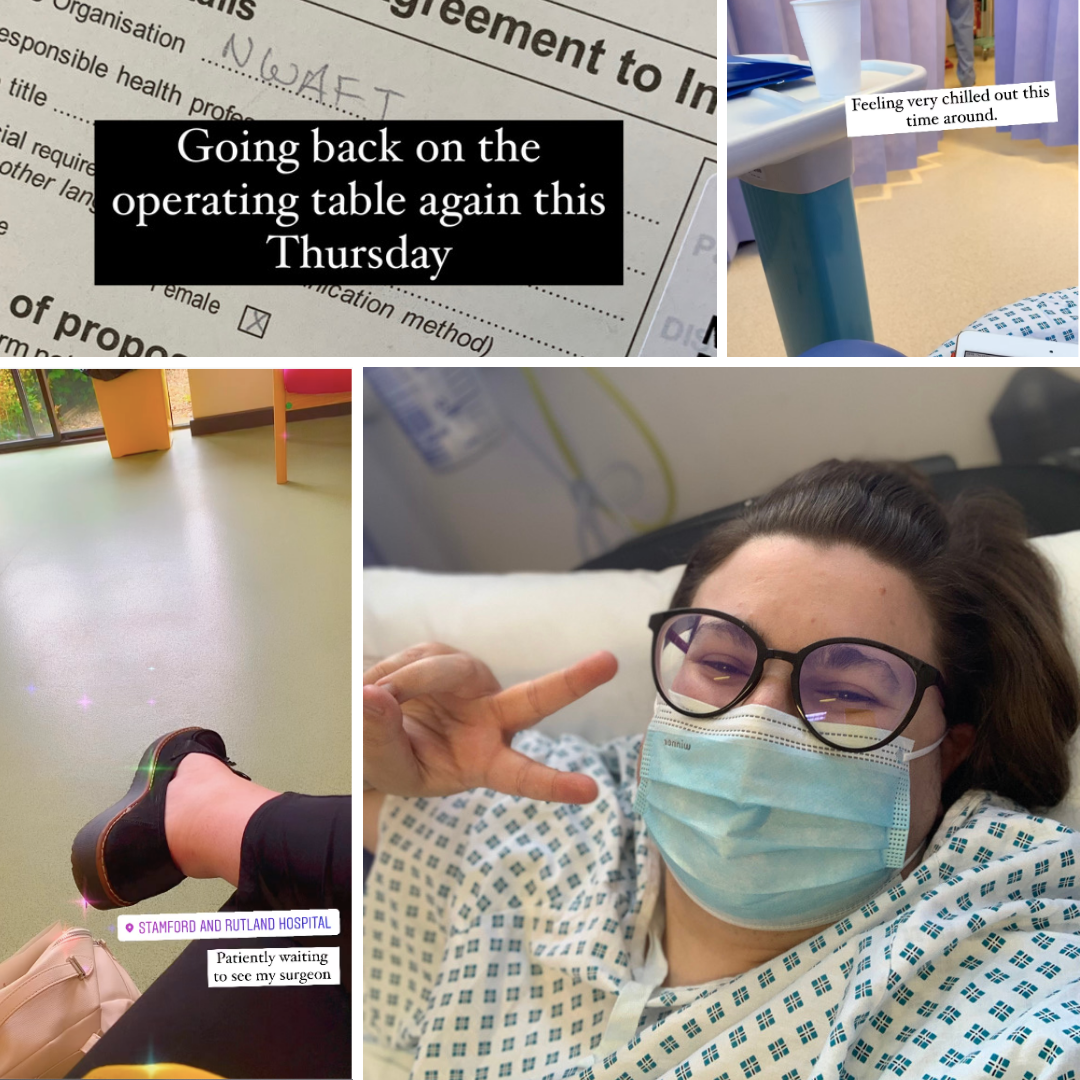
I’ve had three of these examinations under anaesthesia over the past two years. One very soon after my proctectomy surgery back in the Spring of 2019 and two more recently and closer together – June and July 2021.

Experience One
Following a lot of discomfort and pain, I had an MRI to check my proctectomy wound. It was not healed, even though it has been three months and had already been opened up previously during my admission. After a rather quick EUA under GA, I came round, not enjoying any part of having been asleep and was very very sick. I stayed on the Day Surgery ward for the whole day and had a continuation of the daily packing of my wound with my nurse. This would go on for another 8 weeks until my repeat MRI came back with it beginning to close without the need for more intervention.
Experience Two
Over two years since my proctectomy surgery, I attend a regular follow up appointment with my surgeon for my recent hernia repair and I mention an abscess I’d had pop up on my lower right buttock. He examines it but really needs more of a look, as he suspects it’s a tract from my proctectomy wound (which is about an inch left of it). While in surgery for that, he finds a sinus tract that has a cyst in it and removes it. I am left with two wounds. This surgery I had under spinal anaesthesia as I had some issues with my hernia repair. Recovery from this was odd – another whole day on the ward but waking up my legs was very very odd – and daily wound packing began once again.

It brought up all the old feelings of my proctectomy recovery – more daily appointments, more dressings in the house, more showers and careful drying to ensure it heals, more lying down on my sides, not on my butt cheeks. More time off from doing my work, more experiences of taking pain relief to try and get into a rhythm of not feeling awful all day. It was a lot. Some days I really struggled, especially when it was a new person dealing with my wound. I got a good month of appointments with the same nurse which really helped – we could track progress together – until I felt some more pain.
Experience Three
Not so soon after feeling more pain, I happened to have a follow up from the above examination under anaesthesia. He examined me and promptly booked me in for surgery two days later. Covid test, blood tests and consent signed, self-isolation for 48 hrs. This one came as a GA, and I had a surgical drain placed in to keep the wound open so that it would not re-abscess.
This was by far the hardest one. The drain was too long, to begin with, a nurse shortened it and I was much more comfortable. But daily cleaning and checks were mentally draining. Let along travelling there, managing my pain and trying to revise. This surgery lead me to push back an exam because I just could not sit down for longer than 15mins at a time and was really affecting my concentration. After three weeks, the drain came away from the wound site. It wasn’t supposed to but my body was healing by rejecting it – literally.
Since then, I’ve had the wound tended to a couple of times of a week, checked on again by the surgeon and scanned once more when I felt a new abscess coming up. Right now – as if early October – I await a possible examination under anaesthesia with a wound vac and lengthy admission to have specialized wound care.
Tina Aswani Omprakash of Own Your Crohns describes examinations under anaesthesia in a very similar pattern to myself.
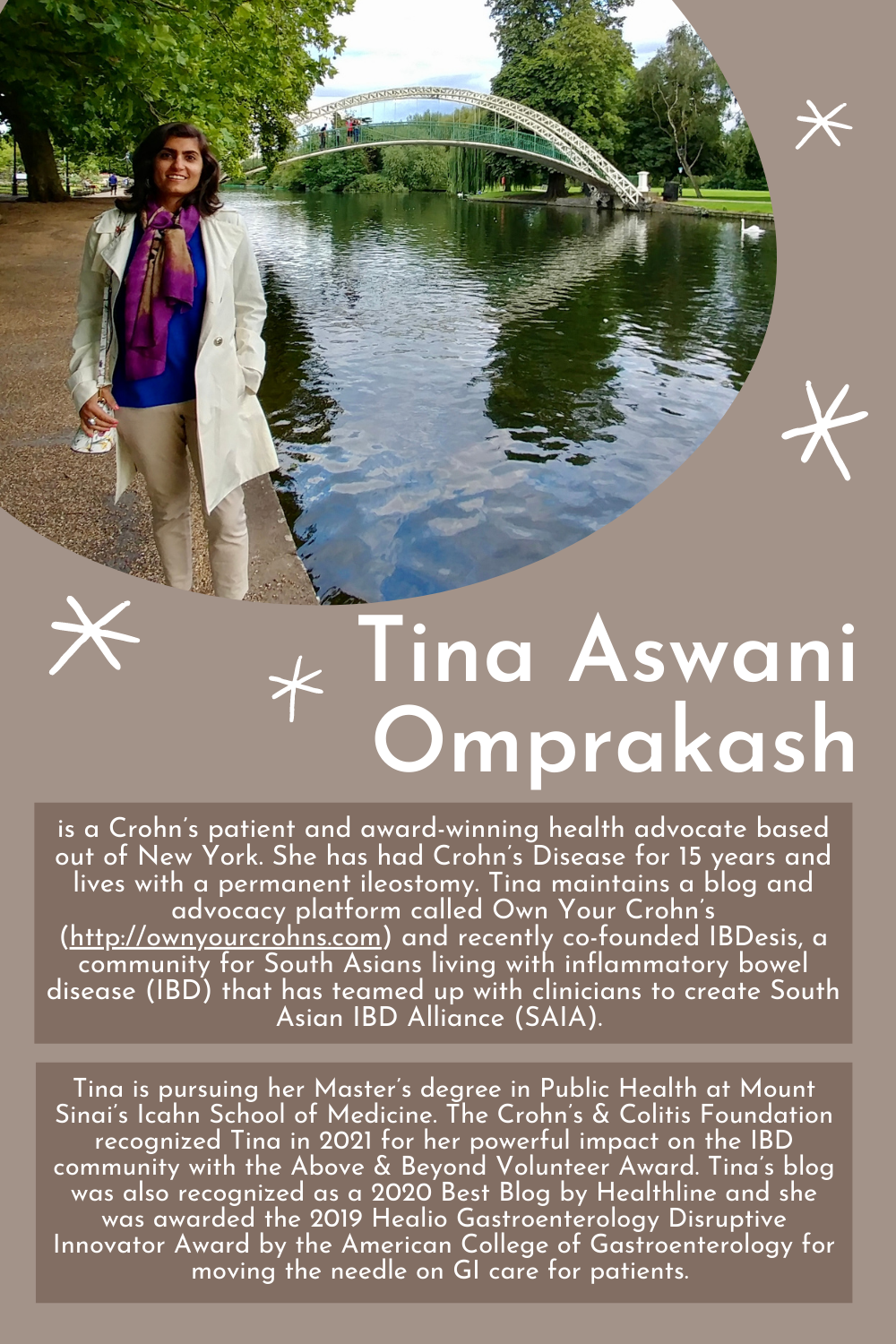
She has “had many EUAs to look at fistulae, to place drains, to curette a non-healing wound” for “perianal Crohn’s disease, j-pouch related issues including pouchitis” after she was originally diagnosed with UC and then had it changed to Crohn’s.
Much like myself, her “recovery was honestly always difficult. EUAs may be basic procedures in a nutshell but for me, they’ve always involved significant trauma in recovery.” The “packing [of] wounds was hard and often on my rear end or vaginal region. I would have to change the packing 3-4x a day to keep it clean and dry. One of the worst procedures I had to have was correcting a j-pouch excision that was done incorrectly. I had to have EUAs every other day to clean the wound & wound-vac out; it was probably the most traumatic experience I’ve had to date. I remember screaming in pain and feeling constant torture and still live with PTSD around it even though I was technically ‘out’ for the procedures.”
Her last examination under anaesthesia was 6 years ago but she recalls how traumatic the at-home recovery was; “[they were] extremely traumatic. And to ask my mom or husband to do it felt quite dehumanizing in many ways and took a toll on my marriage because I didn’t feel quite sexy or attractive anymore. I had to rebuild my marriage many times over after such procedures and it was no joke.”
As with my own experiences, her EUAs were used for different reasons, depending on what the situation called for. She explained “It was and it really depended on what complications I was facing. Now that I’m on a biologic that’s helped control some of the complications of Crohn’s, I haven’t needed it as often. The examinations under anaesthesia were done to help improve my IBD but the path to get there has been excruciatingly painful and difficult. The interventions often break you before they put you back together again. And that’s probably been the hardest thing for me to accept.”
She revealed that she speaks to her therapist about the need for another EUA in the near future; while she feels tired and exhausted, [she is] “working with my therapist to make sure I get ahead of it before it traumatizes me again.” She highlighted how deep the emotional and mental scars go – “I’m still getting over feeling unattractive all these years later.” – just showing that there is a lasting negative impression to EUAs despite their pictured improved quality of life for patients.
Given the intimate nature of examinations under anaesthesia, I’ve found that not a lot of patients know what they actually are unless they have experienced themselves. But even more, patients who could need them within their disease pattern – ie those who have been diagnosed with perianal or vaginal Crohns disease or have manifestations in those areas – can not find anything beyond medical literature to help them understand the reality of a EUA beyond the confines of the hospital.
So, I hope this has helped anyone, someone who might need an examination under anaesthesia in the future. I suspect I am in for a couple more soon so I will continue to explore this subject more as time goes on.
Until next time,

Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
If you enjoyed this post check out Exploring the Emotional Complexity of IBD Surgery and Having Majory Surgery during a Pandemic
You can follow Tina’s advocacy work and read more about her own journey – on Twitter – on her website – on Instagram – on Facebook. She also contributes to South Asian IBD work too on Twitter.