
“Will you always need check-ups for your IBD?”
Short answer: Yes.
Long answer: Yes but here is why:
Getting diagnosed with IBD for most is a great relief. It ends the months, even years, of needing answers but them being dismissed or ignored. But diagnosis is just the first step in a lifetime of appointments, scans, procedures and consults with a specialist team or several teams.
IBD is a chronic, lifelong invisible illness.
Those three words – chronic, lifelong and invisible – mean that it is a) yet to be ‘curable’, b) will be with the patient for their entire life time and c) remains largely hidden from public view.
So, we under go routine check ups with our doctors, our specialist teams and nurses to ensure that we have a current and accurate picture of just what our individual case of IBD is doing. We track progress, we keep an eye on issues and monitor early warning signs. As the years go on, we – as patients – get somewhat used to this pattern of routine appointments to ensure we are doing well – on treatments, in remission or after surgery/surgeries.
But if you are new to IBD, what exactly will become routine? How can I lessen the fear and anxiety around ‘lifelong’ and ‘incurable’ with reassurances about what is ‘expected’?
NB: what I will highlight below are all the possible routine check ups that happen under the sphere of IBD. You may not experience all of them, just some. Some years you might find that things change, and you have more or less of these check ups. Bear in mind, that every case of IBD is invidividual.
What are IBD check ups?
IBD check ups are a combination of clinical evaluation – usually with a gastroenterologist or IBD specialist nurse – to determine if current treatment is working and if any changes are required. They will order further procedures, tests and blood work to check the current status of your IBD.
Why are they needed?
They provide your team with up to date information about how your IBD is. Particular tests can check on particulars in your own case of IBD – ie strictures, fistulae, post surgical complications – and if medications are being effective – ie the balance is correct and the toxicity of some drugs is at an acceptable level.
It will also provide information for patterns and trends to emerge, over time.
What is included?
Diagnosis procedures:
- Physical exam
- Blood work
- Stool samples
- Looking at the gut via endoscopy
- CT or MRI scan

Routine procedures:
- Standard blood work
- Specialist blood work
- Stool sample
- Colonoscopy or Flexi Sigmoidoscopy
- MRI scan of the small bowel
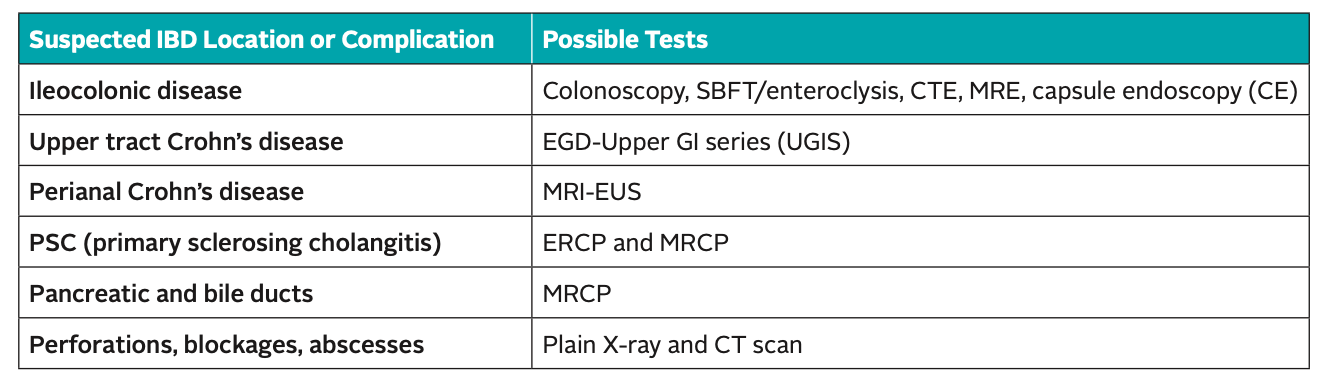
Key to test abbreviations:
- CTE (computed tomography enterography): a variation of the CT scan where the patient swallows special contrast agents to give a sharp outline of the intestines in the X-rays.
- Magnetic resonance enterography (MRE): can give a detailed picture of the small and large intestine, similar to CT enterography.
- MRI EUS – Endoscopic ultrasound (EUS): a technique that uses an ultrasound probe attached to an endoscope to obtain deep images of the gut below the surface. With IBD, physicians use EUS most often to look at fistulas in the rectal area.
- ERCP (endoscopic retrograde cholangiopan- creatography): a type of endoscopy that utilizes X-ray to diagnose a liver disease called primary sclerosing cholangitis (PSC).
- MRCP (magnetic resonance cholangiopan- creatography): a type of MRI that allows the physician to see images of the bile ducts, which are similar to ERCP images.
How often is ‘regular’?
Again, this will dependent on your own IBD. It could be six months or yearly – this time frame is most common with those on medications and post surgical – but it could be longer if you are in clinical remission and without any issues.
And again, it could be one or a combination of any of the above procedures to keep a check on your IBD.
The list in extensive so that it gives clinicians many options to get the best picture – literally and figuratively – of your disease at that moment in time. A combination usually works well – blood and a scan, for example – so they have more than one snapshot to evaluate you with.
NB: it is important to note that, there is always blood work and an endoscopy involved in diagnosing IBD, as a single blood test, a single stool sample or single scope is not conclusive on IBD. That has been set out by the IBD Standards, which is worth a read and available here.
Until next time,

Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
If you enjoyed this post check out Ostomy Glossary and Ostomy Supporting Products – Information
References:
IBD Standards – Regular and Long Term Review – IBD Standards, IBD UK, 2020
Diagnosing and Monitoring IBD – Crohns and Colitis Foundation of America [CCFA], June 2018
Getting a Diagnosis – Crohns and Colitis UK
Managing the long term care of inflammatory bowel disease patients: The cost to European health care providers – James Buchanan et all, Journal of Crohn’s Colitis, 2011




1 Comments
"What does an endoscopy feel like?" •
02/06/2021 at 09:33
[…] enjoyed this post check out “Will you always need check-ups for your IBD?” and Movieprep – The storm before the […]