
“How does sleep affect IBD?”
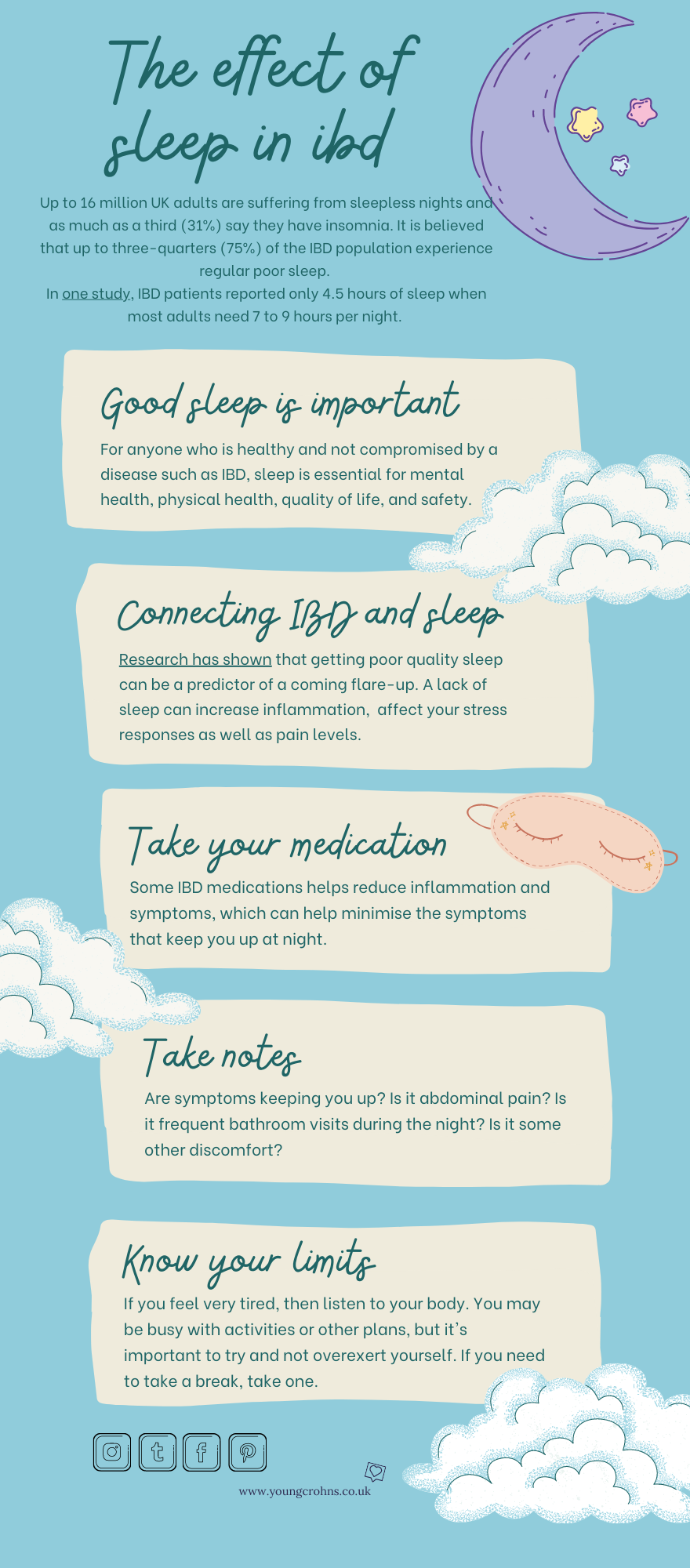
Struggling with sleep is a very common problem. So common in fact that almost one third of the UK population have insomnia – the inability to sleep at night. For those with IBD, I can only image that this proportion is higher, much higher.
When I’ve been in the midst of a bad flare, I would not sleep. I’d be up in the bathroom multiple times during the night, I’d be experience pain – in both my gut and butt – but I’d be absolutely exhausted. you’d think that being so tired, I would just nod off easily. Nope, my head would find it very difficult to switch off – because, at some point, I would be back in the bathroom. Maybe in 10 minutes, maybe in an hour; but I knew I would be. It was an ongoing cycle and I was dependent on caffeine to get me through my workdays. Keep in mind this is while I was waiting for procedures to be completed, results to come in, medication to finally kick in. I wasn’t being neglectful of my condition, it was just part of it. And that makes me sad. Because good sleep is imperative to us as human beings.
In 2014, Crohns & Colitis UK funded research at the University of Bristol which looked into how IBD can affect a person’s ability to sleep. It stated that “Sleep disturbances in IBD are common, increasing during flare-ups but are still present when symptoms have settled down. Studies show sleep problems reduce the quality of life for people living with IBD and reduce their threshold to cope with symptoms such as pain and fatigue. Poor sleep may also worsen IBD by affecting how the body’s immune systems functions.“
The research concluded that “People had problems falling asleep and kept waking during the night. On average people reported only 4.5 hours of sleep a night. Many reasons were given for this lack of sleep including pain, bloating, needing to use the toilet or needing to drink water at night but also feeling anxious about things, including soiling the bed and their lack of sleep.
IBD healthcare specialists recognised the importance of poor sleep in IBD, but not the extent or impact described by patients. Specialists found it difficult to get patients to talk about sleep issues. They felt a little powerless to help, with little to offer apart from basic advice and were not keen to suggest sleeping medications.“
What is the link between sleep and IBD?
Common sleep disturbances included feeling too cold, difficulty falling asleep within 30 minutes, waking in the middle of the night, waking to use the bathroom, having nighttime pain, and using medications to help with sleep.
What does ‘bad’ sleep do to IBD?
One study concluded that “Among 1291 patients whose CD was in remission at baseline, those with impaired sleep had a 2-fold increase in [the] risk of active disease at 6 months (adjusted odds ratio, 2.00; 95% confidence interval, 1.45-2.76); however, no effect was observed in patients with UC (odds ratio, 1.14; 95% confidence interval, 0.75-1.74). These findings persisted in a number of sensitivity analyses.”
CCFA published this article in August 2016 which highlights that “The study found that 77% of the Crohn’s subjects had a PSQI score of greater than 5, which indicates poor sleep… The study also found that: Poor sleep quality is associated with clinical disease activity. Patients with an increased BMI and use of psychiatric medications (non-benzodiazepine) had greater odds of a Pittsburgh Sleep Quality Index (PSQI) score above 5. PSQI score greater than 8 is associated with worsened outcomes, including hospitalization or surgery.”
It went on to suggest that “some studies have found that certain biologic medications – like vedolizumab and anti-TNFs – are associated with sleep improvements.” While another looked at one particular treatment – Cognitive Behavioral Therapy for Insomnia (CBT-I) – as an option to help IBD patients with sleep disturbances, pain, and depression.
What we can conclude from here is that there seem to be lots of data regards IBD and the links to sleep, including the effect that poor sleep hygiene – An overall lack of consistency in sleep quantity or quality, having a hard time falling asleep, experiencing frequent sleep disturbances, and suffering daytime sleepiness are the most telling signs – has on chronic illness. But there are not a lot of answers to fixing the issue.
How can you improve sleep?
At present sleep promoting medications are the only option for people living with IBD.
The new research into CBT-I – as mentioned above – could be the next step towards having this part of IBD care. CBT-I involves: 4-8 visits with a sleep psychologist, sleep restriction therapy, stimulus control, relaxation training, cognitive therapy and sleep hygiene education. CBT-I is a very effective intervention but is underutilized and not always widely available.
- Find a med that works well for you – The goal of IBD treatment is to reduce the inflammation that triggers your signs and symptoms. That’s why finding the medication(s) that works well for you, will help both during the day and at night. The medication you take depends on the area of your colon that’s affected. Medications can control inflammation as well as other symptoms like pain, intestinal bleeding or diarrhoea. Sometimes combinations of medications that act both throughout the body and locally on the intestines can help to improve your overall symptom control.
- Relax– Being anxious or stressed before bed will only make matters worse for your IBD and sleep. Relaxation techniques like deep breathing, meditation and yoga can help your body relax and may ease pain.
- Watch your nighttime eating – Eat larger meals earlier in the day when digestion is easiest. Aim to stop eating at least one to two hours before bedtime. Avoid spicy, fried or heavy meals, which are harder to digest, could help too.
- Shut off electronics – Put away your phone, tablet or computer and turn off the TV at least 30 minutes before bedtime. Sixty minutes is ideal, but 30 minutes is more practical for most. Electronics’ high-intensity lights arouse the brain and may prevent slumber. Before bed, you can do light reading with traditional books, practice meditation or listen to relaxing music.
- Keeping a sleep diary – Keeping note of the different things that are keeping you awake at night or waking you up from sleep is important for identifying any symptoms that need to be addressed.
- Monitor caffeine – Caffeine intake can irritate IBD symptoms and prevent sleep. Know your limits; some people are more sensitive to caffeine than others. Up to 400 milligrams of caffeine per day appears to be safe for most adults, according to the Mayo Clinic. How much is that exactly? It’s about the amount of caffeine in four cups of brewed coffee, 10 cans of coke or two energy drinks.
- Limit naps – Don’t take long naps. Yes, a short power nap can be rejuvenating and help you relax, reduce fatigue and increase mental alertness. But if you sleep longer than 30 minutes, you can feel groggy, and it can be difficult for you to fall asleep at bedtime.

Until next time,

Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
If you enjoyed this post check out Crohns and Colitis Awareness Week – December 4th: Fatigue and Crohns and Colitis Awareness Week – December 5th: Misconceptions
Resources:
Causes of sleep disturbances in IBD patients – Crohns and Colitis UK, 2014
Sleep and Inflammatory Bowel Disease: Exploring the Relationship Between Sleep Disturbances and Inflammation – Jami A. Kinnucan MD, David T. Rubin MD, and Tauseef Ali MD, Gastroenterol Hepatol (N Y). 2013 Nov; 9
Living with IBD – Sleep Addressing poor sleep Crohns & Colitis Foundation
How Sleep and IBD are Related – Very Well Health – Amber J. Tresca
15 Tips for How to Get a Good Night’s Sleep with IBD – Nori Health



