When might you need a Liver Biopsy with IBD?
What does the liver do?
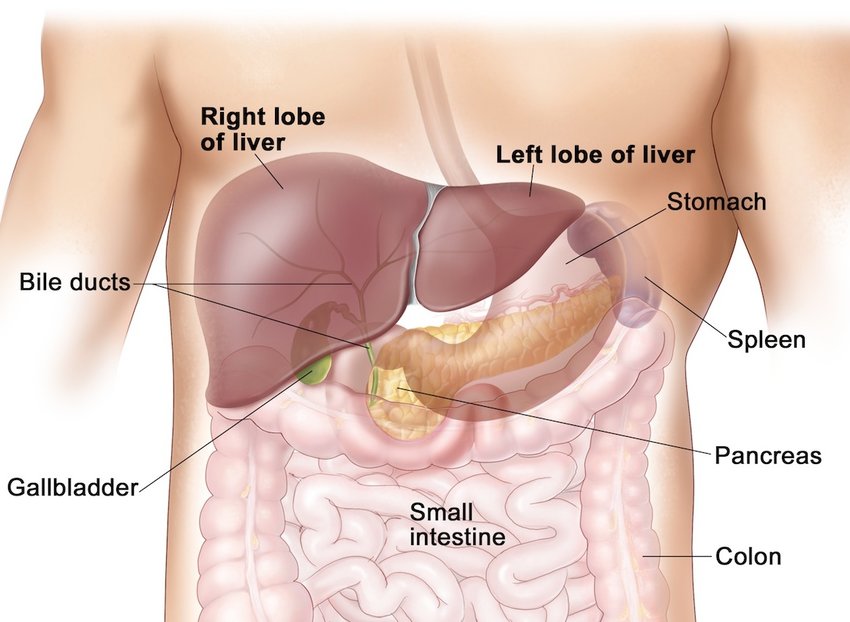
One of the jobs of the liver is to act as a “processing plant,” taking in what we ingest and helping to break it down into waste as well as useable materials. The liver also produces cholesterol, acids, and bile salts that get stored in the gallbladder until required to help break down ingested fats.
How IBD affect the liver?
In some people with IBD, the liver can become inflamed or damaged. Most liver damage is reversible, but the serious liver disease can affect about 5% of people with IBD. Unfortunately, some drugs used to treat IBD may also damage the liver.
Common symptoms of liver inflammation include low energy or fatigue. Many times, patients are asymptomatic. More advanced liver damage leads to a feeling of fullness or pain in the upper right abdomen, itching, jaundice (yellowing of the skin and whites of the eyes), easy bruising, fatigue, and fluid retention. Blood tests can usually confirm the presence of liver disease, although ultrasound, CT scan and MRI scan, as well as other tests, including endoscopic examination of the bile ducts (ERCP) or liver biopsy, may be necessary to confirm the diagnosis.
According to a study published in 2019 by the American Gastroenterological Association, the prevalence of nonalcoholic liver diseases in patients with UC was more than double that of the general population. Considering the increased risk, it makes sense to take precautions.
Common Hepatobiliary Manifestations of IBD
- Hepatic Steatosis – one of the more common hepatobiliary manifestations of IBD found in patients with Crohn’s disease and ulcerative colitis. This is characterised by large collections of fat droplets found within liver cells seen when tissue from a liver biopsy is analysed. Hepatic Steatosis may also be seen with abdominal ultrasound with the liver appearing large and “fatty”. As the IBD improves and better nutritional status is maintained then the fatty infiltration may improve and be reversible.
- Cholelithiasis – or gallstone formation, is the second most frequent hepatobiliary manifestation of IBD and is more common in Crohn’s disease than ulcerative colitis. Gallstone formation occurs when there is a diminished absorption and resecretion of bile acids. Bile salts keep cholesterol in solution and if they are decreased in amount cholesterol precipates forming gallstones. These stones collect in the gallbladder and cause inflammation or distension, which can result in severe pain in the upper right hand side of the abdomen. An abdominal ultrasound will determine the presence of gallstone formation.
- Hepatitis – a generic term for inflammation of the liver. It can be caused by medications like methotrexate, azathioprine, 6-mercaptopurine (6MP) or rarely anti-TNF agents. Your doctor will do periodic blood tests to monitor for this condition. Hepatitis can also be caused from inflammation of the liver itself related to a person’s IBD, called autoimmune hepatitis. It is treated with the same kinds of medicine that ulcerative colitis and Crohn’s disease are treated with, to decrease the inflammation. Autoimmune hepatitis can lead to liver scarring (cirrhosis) and permanent liver damage if not treated. Hepatitis can also be from viruses like Hepatitis A, B, or C and should be treated the same as in patients without IBD.
- Primary Sclerosing Cholangitis (PSC) & Pericholangitis – two relatively uncommon manifestations of IBD. These hepatobiliary diseases are characterized by inflammation and/or scarring of the bile ducts within the liver (intrahepatic) and outside of the liver (extrahepatic). Primary sclerosing cholangitis occurs in approximately 1-5% of patients with IBD. It is more common in males than females, and is more frequently associated with ulcerative colitis than Crohn’s disease. Primary sclerosing cholangitis may cause narrowing of the bile duct and the development of jaundice. On the other hand, pericholangitis occurs in approximately 30% of patients with IBD. This consists of inflammatory cells surrounding the small bile ducts within the liver but there is no damage to the liver cells or to the bile ducts, and does not usually progress to more serious disease.
What has been my experience?
My liver issues have been going on since 2014 when I ended up in A&E from a stomach bug and my LFTs (Liver Function Tests) were well beyond the upper parameters! It was quite a shock, as I’d only had my routine IBD blood monitoring done a week or so before.
I was referred to a Hepatologist via my GI at the time, and went through a battery of detailed blood work to pinpoint the problems origin and got a couple of tests done too. This took about a year, going back every 3 months to get a better picture of why my liver tests continued to be high, despite going down from the highest value in 2014.
He finally concluded that I had NFLD – Non-Fatty Liver Disease – and just needed to have my liver tests repeated each time I had my bloods done for my monitoring on my biologic medication. I’d gone from Infliximab, to Inflixmab with Methotrexate to Vedolizumab in the time I was seeing my liver specialist, and no change was really seen. So we ruled out it being medication-related, it was in addition to IBD. Or, maybe I’d had it all along and it just popped up. We’ll never know for sure.
Since then, I’ve had both my subtotal colectomy and proctectomy surgeries and both of those results in my LFTs rose beyond a level my IBD team felt comfortable with and referred me to the hospital Hepatologist who has a second speciality in IBD related liver issues. She repeated all tests, do a fibroscan – to check for fatty deposits in my liver via Ultrasound – but finally wanted to do a liver biopsy.
This took place in February 2019. It was pretty straightforward and not at all uncomfortable. It was small day surgery and took less than 30 mins. Resting afterwards took the longest time, as you can’t lie on your right-hand side to avoid liver injury or bleeding. This biopsy concluded that my NFLD was indeed correct and we would only need to monitor it. It has been pretty much under control since then, occasionally, ill have a high liver result come back but we always have the option to go back to the Hepatologist for advice.






Until next time,
Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
References & Further Reading:
- Canadian Society of Intestinal Research – IBD and Liver Disease
- Crohns and Colitis Foundation – Liver Disease Fact Sheet
- Liver Disorders in Inflammatory Bowel Disease – Victor Uko, Suraj Thangada, and Kadakkal Radhakrishnan, Gastroenterol Res Practice 2012 Feb 15
- EveryDay Health – Liver Conditions Linked to Ulcerative Colitis