
“Are supplements helpful in IBD?”
More than half those with IBD have deficiencies in vitamins & minerals and we get most of these from the food we eat. Clemmie Oliver of the NALM Clinic said it best; “micronutrient deficiency (vitamins and minerals) is associated with a prolonged and more complicated course of disease in people with IBD as micronutrients play hugely important roles in our bodies, including supporting and regulating our immune system, gut health and energy levels, so correcting any deficiencies, and supporting nutrient intake should always be an important consideration in the management of IBD.”
The pure fact of living with a gut disorder such as Crohns disease or Ulcerative Colitis means that our bodies simply do not absorb key nutrients due to the fact we can suffer from:
- chronic diarrhoea
- blood loss
- have extensive bowel surgeries
- endure potent medications as treatment options
So, for the general public – who fit, healthy and eat a balanced diet, supplements are a big fat NO. For those people, they can at the very least pricey and wasteful, on the other end of the scale – harmful to the delicate balance of nutrients needed by the body to function.
Deficiencies in IBD
Common deficiencies in IBD can be:
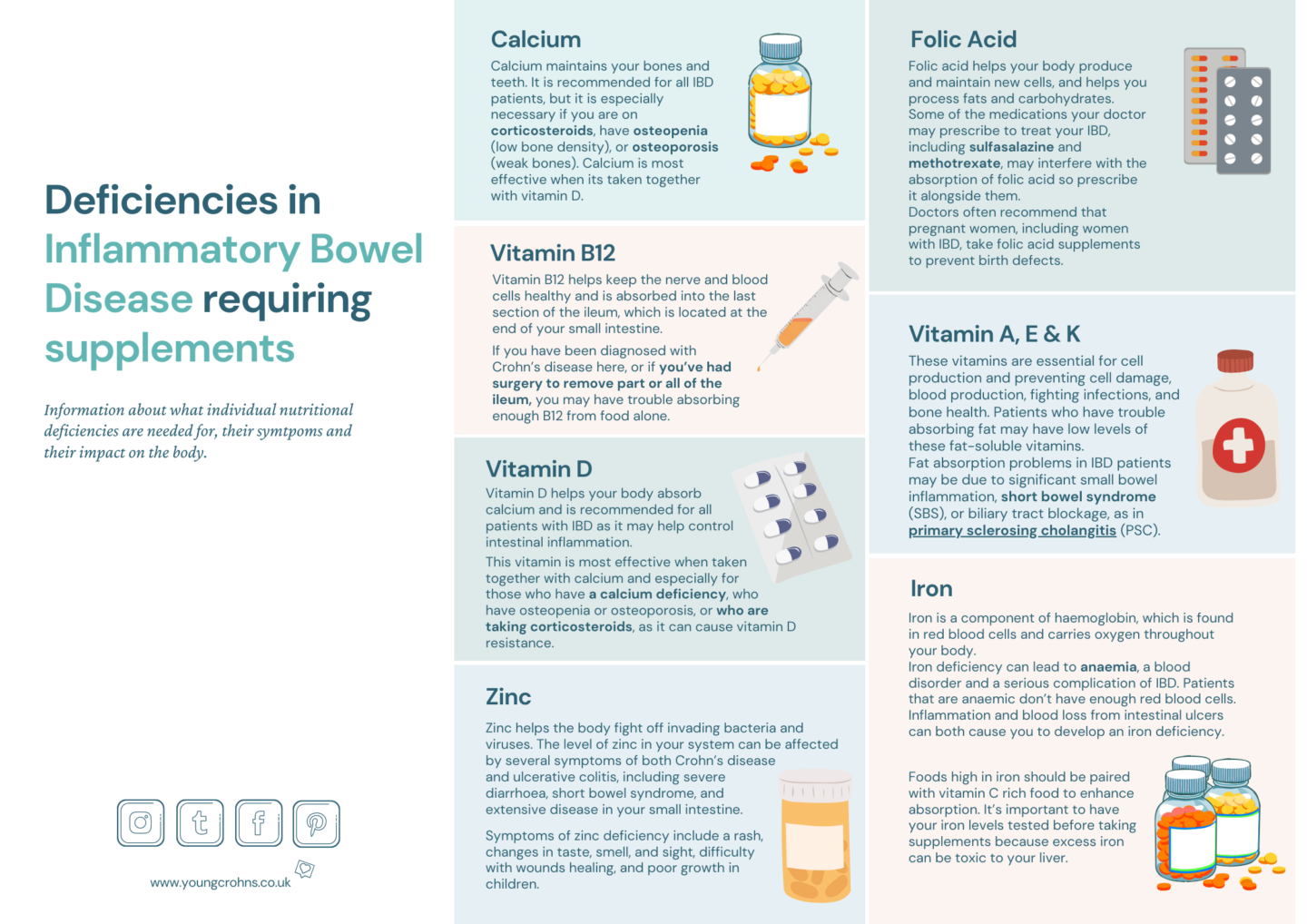
Deficiencies are more common in Crohn’s disease as the small intestine – where we absorb most vitamins and minerals – is involved. There are also more noticeable during flare-ups but can have prolonged effects in remission too. The above poster gives an indication as to where these nutrients are absorbed related to your own particular location of the disease.
Requirements for needing supplements
- extensive disease in particular locations of the intestine, most likely the small intestine.
- restricting food intake
- blood loss
- severe or chronic diarrhoea
- surgery – any which removes small intestine
- diagnosis in children and pre-teens – before growth development
Most times, requirements of additional supplements are diagnosed after consultations with a gastroenterologist or dietician who order extensive blood work to get levels of particular deficiencies. From that, they will recommend dietary additional to help bolster the nutrient you take in through food, but can also prescribe supplements in tablet or liquid form.
NB: Some IBD teams are more proactive and reactive with deficiencies, whereas others might need a gentle nudge or reminder to carry out regular blood work to check things such as Vitamin D, B12 or iron levels.
Benefits of prescription supplements
- Specially guided by a clinician.
- Correct dosage, regiment and treatment length.
- Reviewed regularly.
- Only can be authorised by an HCP.
Benefits of supplements Over The Counter [OTC]
- Readily available.
- Usually on offer – either under an umbrella 3 for 2 from Boots or large supermarkets or the ‘Buy a second for a Penny’ offer from Holland & Barretts.
- Should only be used if it comes as a recommendation from a clinician.
So, what should we do? NALM Clinic recommend:
1. “Food first – we know the best way for us to get nutrients is through the food so aim for a balanced plate of protein (e.g. meat, fish, eggs, beans, legumes, chickpeas, lentils, quinoa etc), carbohydrates (e.g. potatoes, root veg, grains, fruit, vegetables) and healthy fats (e.g. yoghurt, cheeses, nuts, seeds, avocado, olives, oils). Focus on the colour and variety of fruits and vegetables, and opt for whole grains.
2. Worried about a deficiency? – Go to your GP, gastroenterologist or nutritionist and get a blood test done to check. If you are deficient, we also need to look at WHY that might be – Poor diet? Lifestyle? Or is there an underlying problem that needs investigating?
3. Get help – don’t just self-medicate – get help and advice from a nutritionist to make sure you are supplementing correctly and not wasting your money or doing yourself harm.”
Until next time,

Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
If you enjoyed this post check out Iron Deficiency & IBD, The What and Why: Calcium, The What and Why: Vitamin D and The What and Why: Vitamin B12
References:
Crohns & Colitis Foundation – Vitamin and Mineral Supplementation
NCBI: Gastroenterology Clinics of North America, Volume 46, December 2017 Vitamins and Minerals in IBD – F K Ghishan and P R. Kiela
IBD Relief – Vitamin supplements and IBD
NALM Clinic – Supplements – should we all be taking them? (10/2/2020) Nutrient deficiencies & why they should be an important part of IBD management (8/6/2020)



