
Flare Up Management
How to make decisions to help tame the IBD monster
NB: This had been intended to be written before we knew anything about coronavirus (COVID-19) so there has been the addition of COVID information throughout this article; to be relevant and highlighted for easy visibility.
Hospitals are undergoing significant changes as they adapt and respond to coronavirus. This means there have been changes to outpatient clinics and adjustments to local IBD Team Advice line support – so please keep this in mind if you are seeking advice.
If you have a written personalised care and support plan or your IBD team have agreed with you previously what to do if your symptoms get worse please follow the specific guidance given by your doctor or nurse.
If you do not have a personalised plan contact your local IBD Team Advice Line via telephone or email.
NHS guidelines currently advise people to stay home and avoid attending GP, pharmacy or emergency/urgent care services, unless you have been advised to do so. But you will know your body and condition better than anyone. If you feel you need emergency or urgent care telephone 111.
If you have Crohn’s Disease or Ulcerative Colitis and you’re worried about coronavirus (COVID-19), please read the Crohn’s and Colitis UK FAQs which are regularly reviewed and updated.
What is a flare-up?
A flare-up is when symptoms come back and you feel unwell. It will be very personal to you. The symptoms will vary from person to person, over time and will depend on where Crohn’s or Colitis is in your gut.
Signs of flare-up can include:
- Going to the toilet more than 5 times in 24 hours – or more than is normal for you
- Loose stool or diarrhoea with any blood or mucus for more than three days
- Abdominal pain
- Just generally feel worse, especially if you have a fever
- Waking up at night to go to the toilet
You may also experience symptoms outside the gut during a flare-up such as:
- Joint pain and swelling (arthritis)
- Swelling in the eyes
- Mouth ulcers
- Skin rashes
- Fatigue
- Mental health problems
Having a flare-up – what should you do?
- If you have a written personalised care and support plan or your IBD team have agreed with you previously what to do if your symptoms get worse please follow the specific guidance given by your doctor or nurse.
- If you do not have a personalised plan contact your local IBD team Adviceline via telephone or email.
- If you do not get a response from them – beyond what is expected during their working hours and the usual length of turn around – contact your GP practice for medical advice.
- If you feel very unwell, and you have done all you can at home to manage your symptoms, you can ring NHS 111 for advice or attend A&E.
Seeking help from your GP
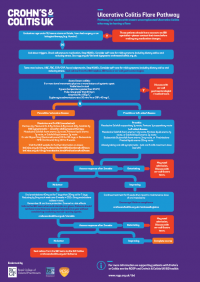
Crohn’s and Colitis UK and the Royal College of General Practitioners (RCGP) created the ‘Inflammatory Bowel Disease Toolkit’ in 2019 to help aid GPs in giving IBD patients standard access to primary and secondary care during a flare-up.
“GPs are often the first person people with Crohn’s or Colitis will turn to when having a suspected flare, yet 52% are less than confident or not confident if a patient visits their clinic with a flare-up. The new flare pathways provide advice on steroid intervention, dose escalation, and when to refer to secondary care. This promotes shared care between GPs and hospitals, meaning suitable patients can be appropriately managed in primary care with rapid access to advice from the IBD team if is needed. It aims to give both GPs and patients confidence to know what to do when in a flare.”
When should I seek urgent or emergency care?
NHS guidelines currently advise people to stay home and avoid attending GP, pharmacy or emergency/urgent care services, unless you have been advised to do so. But you will know your body and condition better than anyone. If you feel you need emergency or urgent care telephone 111.
Some signs could include:
- Stoma blockage: not passing wind or stool, or passing watery stool, nausea, bloating or swelling tummy, tummy cramps, swollen stoma, nausea/vomiting or both.
- Severe dehydration, malnourishment and vomiting.
- Severe tummy pain, a high temperature and a rapid heartbeat.
- All medicines have a small risk of side effects, such as chest pain, rapid heartbeat or hives. If you experience any side effects that you are worried about while taking your medicine, contact your IBD team or your GP as soon as possible.
Staying well with IBD
It is important to feel empowered to manage your condition. Crohn’s and Colitis UK’s information resources and videos give a wealth of advice on how to manage symptoms, stay as well as possible and where to find emotional and peer support.
Top tips for keeping as well as possible are:
- If you don’t have symptoms of coronavirus, continue taking your medication as normal unless your doctor or nurse have advised you otherwise.
- Ensure you have a good supply of medicines should you need to self-isolate or shield yourself.
- Stay hydrated. If you are flaring and experiencing diarrhoea, it’s important to make sure you are drinking enough to replace what you have lost, and in doing so getting the right balance of sugars and essential salts into your body to keep hydrated.
- Eat well. Living with Crohn’s or Colitis may mean making some changes to your diet. You may need to avoid certain foods to help your symptoms or take extra care to make sure you’re getting the right nutrients. There’s no single diet that works for everyone – but there is a wealth of good information that can help you understand how food affects your condition, so you can make the choices that are right for you.
- Take rest and sleep. Here are more tips on pacing, exercise and managing fatigue
- Wash your hands frequently and avoid touching your face.
- Quit smoking as this increases the risk and severity of COVID19 infection.
- Avoid NSAIDs (non-steroidal anti-inflammatory drugs) such as ibuprofen.
- Protect your emotional and mental well-being. There are a number of excellent resources being produced to support people during Coronavirus from organisations like MIND and the Mental Health Foundation. However, if you are struggling with your Crohn’s or Colitis and would like to talk to someone, there is information on IBD and counselling.

Further Reading:
Crohns and Colitis UK – New Flare Pathways Launch to help GPs
IBD UK – IBD Standards – Flare Management – Flare Pathways
Do you have any questions or queries? Or just want to share your own experiences?
You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram

If you enjoyed this post check out ‘I try real hard but I can’t forget’ , One. Year. Ago. Today. and A Spiral of Set Backs




3 Comments
thedailytrotter
24/11/2020 at 15:36
Fabulous post. Great advice for managing symptoms and where to turn
Admin
24/11/2020 at 16:30
Thank you! Glad you enjoyed it 🙂
"Can having IBD be painful?" •
23/06/2021 at 16:48
[…] If you enjoyed this post check out Pain: When does Acute turn into Chronic? and Flare up Management […]