
IBD v IBS – Why Do So Many Get “Mis” Diagnosed?
Let’s talk about the similarities and differences between IBS and IBD and why so many get ‘mis’ diagnosed with IBS.
First of all, what is IBS?
IBS stands for Irritable Bowel Syndrome. It causes cramping, bloating and pain in the large intestine or the colon. It is very common and is linked with food and stress triggers. There is no one cause for IBS but it is managed through changes in diet and reduction in stress levels.
Then what is IBD?
IBD stands for Inflammatory Bowel Disease. IBD is a group of inflammatory conditions that can affect the entire digestive system. Whilst they can also present with cramping, bloating and pain in the abdomen, they also come with diarrhoea or constipation, rectal bleeding, anaemia and dramatic and sudden weight loss. Crohn’s Disease and Ulcerative Colitis are the most common types of IBD; UC affects the colon exclusively where as CD can affect anywhere in the digestive tract from mouth to anus. These conditions are thought to be auto immune disorders – in which the immune system overreact to inflammation, causes ulcers throughout the bowel lining wall. Usually the treatment is medication to control the immune responses to inflammation or even surgery.
How are these two conditions similar?
- Abdominal pain
- Diarrhea
- Abdominal cramping
- Nausea, and/or vomiting
- An urgent need for a bowel movement
How do they differ?
Symptoms unique to IBS are:
- Changes in bowel movement
- Changes in how the stools look
- Abdominal bloating
- Whitish mucus in the stool
- A feeling of not having finished a bowel movement.
- Sexual dysfunction
- Fibromyalgia
- Urinary frequency and urgency
Some people with IBS have IBS-D in which diarrhea is one of the primary symptoms, or IBS-C in which constipation is one of the primary symptoms.
Symptoms unique to IBD (Crohn’s disease and ulcerative colitis) are more serious, and include:
- Anemia
- Eye redness or pain
- Feeling tired
- Fever
- Joint pain or soreness
- Skin changes
- Unintended weight loss
- Loss of appetite
- Rectal bleeding
How are they diagnosed?
Initially, it is difficult for doctors to diagnose IBS and IBD because sometimes some of the symptoms are similar, as shown above. However, whilst this remains true, the fundamental difference between IBS and IBD is that IBD is structural, and IBS is not.
By “structural,” it means that when examining the gut by x-ray, endoscopy, surgery or biopsy it can be seen to damage the structure of the gut. In IBD, this damage is caused by an inflammation whose origins are poorly understood, but whose consequences may require hospitalisation, heavy-duty medication, nutritional support, and often surgery.
In IBS, none of the above statement is true. Examination of the gut of a person who has IBS will be unrevealing. IBS exists because patients have gut symptoms, and there is no other way to detect it.
Correct diagnosis is KEY
What is most important in diagnosis is the Fecal Calprotectin stool test. If the test finds a large amount of calprotectin present in the stool, it is more likely that the patient has IBD, while if the test comes back with low or normal levels of calprotectin, it points more toward IBS.
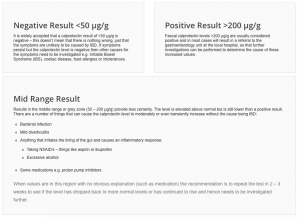
This test is also helpful for individuals already diagnosed with IBD, as it can identify the level of inflammation. If a person diagnosed with IBD subsequently shows low levels of fecal calprotectin, this means that the inflammation is being controlled, so the treatment regime is working.
NB: it is important to note that fecal calprotectin alone will not diagnose IBD. It’s result can rule out IBS but further testing of blood work and endoscopy will be needed to determine the form of IBD and thus its best treatment.
Why have so many been misdiagnosed?
- Lack of education – until recently, IBD was something that wasn’t very much heard about. Now it has much more public awareness, it is spoken about freely in the media, the taboo of speaking about poo has lessened.
- They present very similarly – without a thorough physical exam and full medical history; it can be difficult to see what is most important. And realistically, this can not be done in a 10 minute appointment with a GP.
- Some GPs don’t really look into the results of calprotectin – even if a stool sample is done, the results are sometimes not examined in closer detail.
- GP haven’t always seen much of IBD – as most cases get diagnosed in hospital and treated under a specialist, some GP’s only see the repeat medications coming through, not the patient. It must be hard to know more about it if you don’t see the beginnings of IBD, so its easy to assume its IBS when the symptoms present. This only fuels the circle of lack of knowledge and being able to see it to diagnose it.
- Lack of tools for GPs – CCUK have worked hard to extend knowledge and awareness to GP’s at a local level with their GP toolkit. The RCGP – Royal College of General Practitioners – have also come on board. The toolkit gives GPs access to the pathways to help IBD patients manage their condition; either as newly diagnosed or well seasoned patients.
It is crucial that the IBD symptoms in patients are not confused or dismissed as IBS symptoms. There are many reported instances where IBD has been “misdiagnosed” as IBS for years until finally the diagnosis is made. A likely explanation is that IBS was present first – remember it is very common – and the IBD started later.
Unlike IBD, IBS isn’t classified as a true disease. Instead it’s known as a ‘functional disorder’ meaning that the symptoms don’t have an identifiable cause.
IBS may be treated with certain medications such as intestinal antispasmodics like Hyoscyamine or Dicyclomine. Dietary and lifestyle changes seem to help the most. People with IBS should avoid aggravating their condition with fried and fatty foods and caffeinated beverages.
IBD treatment depends on the form diagnosed. The primary goal is treating and preventing inflammation. Over time, this can damage the intestines. The use of powerful, often expensive, sometimes-toxic drugs employed to treat IBD will hopefully reduce the need for surgery but early diagnosis is also a big factor.
Finally, both IBD and IBS can be mistaken for other diseases such as appendicitis, diverticulitis, and chronic gut infections. Careful attention to the medical history and a thorough physical examination should avoid any such confusion.

Sources:
IBS vs. IBD: What Are the Differences Between Symptoms?
Crohns And Colitis Foundation – IBD & IBS – Similiarities & Differences
EveryDay Health – Irritable Bowel Syndrome: How to Avoid an Incorrect Diagnosis
Gastrointestinal Society – The Irritable Gut: IBS v IBD Whats the Difference?
Healthline – Irritable Bowel Syndrome vs. Inflammatory Bowel Disease
Gastrointestinal Society – Fecal Calprotectin Test
Crohn’s and Colitis UK – NEWS: IBD toolkit for GP’s now Live (7th September 2017)
Royal College of General Practitioners – Inflammatory Bowel Disease Toolkit


4 Comments
Ostomy Uncovered – How to Resize Your Baseplate •
11/01/2021 at 16:30
[…] you enjoyed this post check out IBD v IBS – Why Do So Many Get Misdiagnosed , The Liver & IBD and The What & Why: […]
Fibre with IBD •
03/04/2021 at 21:39
[…] you enjoyed this post check out IBD v IBS – Why Do So Many Get Misdiagnosed , The Liver & IBD and The What & Why: […]
Sleep with a Stoma •
03/04/2021 at 21:42
[…] you enjoyed this post check out IBD v IBS – Why Do So Many Get Misdiagnosed , The Liver & IBD and The What & Why: […]
Crohns & Colitis Awareness Week – December 5th: Misconceptions •
04/04/2021 at 12:45
[…] For some this can be the fact that at a primary level, IBD is confused with IBS. And whilst yes they both are located within the digestive system, that is the end of the similarities. I’ve written about this before, here. […]