Extra Intestinal Manifestations and their Importance
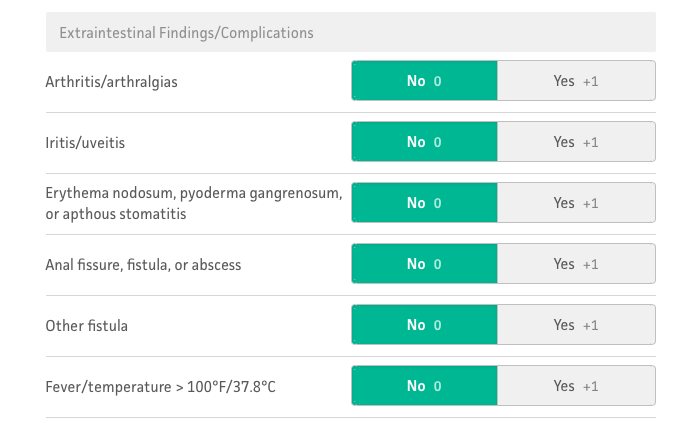
Extra Intestinal Manifestations – or EIMs for short – are seen in 25–40% of IBD patients.1 Inflammatory manifestations of the skin, eyes, liver, and joints are considered primary manifestations. If secondary effects of disease activity are also considered, nearly 100% of IBD patients have an abnormality outside of the gastrointestinal tract.2 Twenty-five percent of IBD patients have more than one EIM. The development of the first EIM appears to increase the risk of developing a second EIM.3
Most IBD patients with EIMs have colonic inflammation, although some patients develop EIMs prior to the onset of colonic symptoms.
Musculoskeletal pain occurs in 9–53% of IBD patients and is considered the most common EIM.1,2,4 The differential diagnosis of this condition includes articular, periarticular, and muscular involvement; osteoporosis and related fractures; and fibromyalgia.
THE SKIN – Major dermatological manifestations have been reported in 2–34% of IBD patients.13 A broad spectrum of skin diseases may occur, and patients may develop multiple dermatological manifestations concurrently during the natural course of their disease.14 Erythema nodosum (EN) and pyoderma gangrenosum (PG) are the most common cutaneous manifestations.13 Other skin lesions include psoriasis, oral aphthous stomatitis, and Sweet syndrome. A dermatological evaluation is mandatory for any of these disorders to help confirm the diagnosis and assist in management.
THE EYES – Ocular manifestations occur in 0.3–5% of all IBD patients.30 Patients with colitis or ileocolitis are affected more frequently than patients with isolated small-bowel disease. An immune complex hypersensitivity reaction to a colonic antigen has been postulated as an explanation for this difference in incidence.31Ocular complications often present concurrently with other EIMs, particularly peripheral arthritis and EN.
THE LIVER & KIDNEYS – Nephrolithiasis, obstructive uropathy, and fistulisation of the urinary tract are relatively common EIMs, occurring in 6–23% of patients with IBD.35 Secondary amyloidosis is a rare systemic complication that involves the kidneys. Patients can present with proteinuria, renal failure, and uremia. Studies have shown a 3-fold increased risk in males and a 10-fold increased risk in CD patients (over UC patients).36 In the majority of patients, other EIMs develop concurrently. A diagnosis can be made with a liver, rectal, or renal biopsy.
EIMs are very common in both UC and CD patients. Generally, we recommend early involvement of specialists in the management of involved organ systems. Most EIMs parallel disease activity and will respond to treatment of underlying bowel disease; however, some diseases, such as PSC, warrant lifelong monitoring of extra intestinal systems. Clinicians must promptly evaluate complications that can cause emergencies, such as uveitis and cholangitis.
Can extra intestinal manifestations of IBD be treated in the same way they would be if they occurred on their own? No. It is important to recognise that these manifestations should not necessarily be treated with traditional therapies. If someone has arthritis, it is natural for that person to consider taking ibuprofen or another anti-inflammatory medication. However, these drugs can be very irritating to the lining of the gastrointestinal tract and may even cause a flare of the underlying IBD.
Treatment for extra intestinal manifestations of IBD should focus on medications that are used primarily to treat bowel inflammation. Acetaminophen and similar drugs can help relieve joint pain in the short term, but pain medications do not treat the underlying inflammation. Once the bowel inflammation is treated with appropriate medications, often the arthritis resolves as well.
Do you advise patients to be on the lookout for extra intestinal manifestations? Yes. Education is a very important tool here. When a patient is newly diagnosed with IBD, I enquire about any previously experienced extra intestinal manifestations. Many patients note such issues but had never made the connection to IBD. Even when there is no prior extra intestinal manifestation, I discuss the possible signs so that patients know to call me if they arise. This counselling is very useful because when issues do occur, patients know to call, and then the problem can be resolved efficiently.
Can some IBD medications also cause extra intestinal side effects? Yes. We consider these issues under a separate umbrella. Therapy-induced complications can manifest in the skin, for example. One example is psoriasis, which can occur as a result of anti-TNF medications. For the most part, the psoriasis can be managed with topical agents, and the primary anti-TNF therapy can be continued. However, sometimes the anti-TNF agent needs to be stopped in order to resolve the skin lesions. Additionally, some therapies, such as azathioprine and anti-TNF agents, are associated with an increased risk of non-melanoma skin cancer. Anti-TNF agents also are associated with an increased risk of melanoma. For these reasons, I counsel patients using these medications to wear sunscreen and have dermatological evaluations. It is important for clinicians to be aware of these problems, too, and to differentiate them from the extra intestinal manifestations resulting from the IBD itself so that appropriate treatment can be provided.
Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram

If you enjoyed this post check out IBD v IBS – Why Do So Many Get Misdiagnosed , The Liver & IBD and The What & Why: Dehydration
Further Reading:
- Extra Intestinal Manifestations – The Joints
- Extra Intestinal Manifestations – The Skin
- Extra Intestinal Manifestations – The Eyes
- Extra Intestinal Manifestations – The Liver
- Extra Intestinal Manifestations – The Bones
- Extra Intestinal Manifestations – Overview
- Erythema Nodosum – My Extra Intestinal Manifestation