Extra Intestinal Manifestations – The Bones
Disclaimer: This information is based on my own research into this particular extra intestinal manifestation of IBD as well as some personal experience and should not be used as medical advice or a diagnostic tool. The suggested investigations and prevalence are part of the IBD protocols set out by NICE; but do vary between CCGs and then thus individual NHS Trusts and specific hospitals. If you seek advice regarding the things you experience within your own disease, please contact your IBD team for medical advice.
This new series looks at the effects IBD can have beyond the gut. As a whole, extra intestinal manifestations of IBD occur when the disease is not controlled well enough with conventional medications. However, the side effects of particular medications can produce new symptoms which would mirror or mimic these extra intestinal manifestations (EIMs). For all of the information provided in this series, I have gathered resources and broken them down, putting them into patient speak. Each post comes with a disclaimer too (see the end of the post) so if you have concerns, you should see your specialist in all instances.
The Bones
Although bone seems as hard as a rock, it’s actually living tissue. Throughout life, old bone is removed and new bone is added. These two processes – bone resorption and bone formation – are twin components of the body’s continuous bone turnover known as bone remodeling. If bone resorption and formation occurred at exactly the same pace, bone mass would remain the same. But that isn’t the case. After age 35 or so, bone resorption outpaces formation and bone density begins to decline. Some loss of bone density is normal. Only when the process accelerates does osteoporosis become a threat.
This post looks at the following:
- Osteoporosis – which means ‘porous bones’ – the struts of bone that make up the inner honeycomb-like structure become thin, so the bone becomes fragile and breaks more easily.
- Osteopenia. This is a mild loss of bone density not severe enough to be labeled as osteoporosis. Research suggests that almost half of all people with Crohn’s or Colitis have Osteopenia.
- Osteomalacia. This is a softening – decalcification – of the bones usually caused by lack of vitamin D. Osteomalacia in growing children is known as rickets and can lead to bone deformity, in adults it can cause pain.
- Ostenecrosis. This is caused by a reduction in blood supply to a bone, such as a hip, and can result in the death of bone and the surrounding cartilage. This sometimes causes pain and stiffness but may have no symptoms. Osteonecrosis – also known as avascular necrosis – is a rare but serious condition and can be a complication of steroid treatment.
Who is affected?
As many as 30% to 60% of people with Crohn’s disease or Ulcerative Colitis have lower-than-average bone density. In some individuals, it takes the form of osteoporosis. In others, the bone abnormality is osteopenia or osteomalacia. These conditions occur more frequently in people with Crohn’s disease than in those with Ulcerative Colitis.
Symptoms
Although people with Osteoporosis may notice some back pain or change in posture, the disorder generally produces no symptoms until the bone becomes so weakened that it breaks. Bone fractures due to osteoporosis most often occur in the spine and hips. This is why screening tests for bone loss – also know as bone density testing – and preventive measures to halt bone loss are so important.
Diagnosis
Diagnosis of bone loss is generally made with a special X-ray technology called dual-energy X-ray absorptiometry (DEXA). Results of the test – which measures the bone mineral density in the spine, hip, and other bones – indicate the risk of suffering a bone fracture. In the general population, a diagnosis of osteopenia doubles the risk of fracture; osteoporosis increases the risk by four or five times. But here is an interesting recent finding: Although people with IBD have above-average rates of osteoporosis and osteopenia, their actual fracture rates are comparatively low.
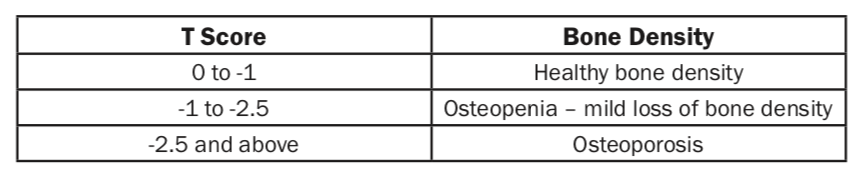
The results from a DXA scan are used to work out a bone density score. Your bone density is compared to that of an average healthy person in their 20’s and is known as a T score.
You are most likely to be offered a DXA bone scan if you have Crohn’s or Colitis and other risk factors such as:
- a woman after the menopause
- a woman who has had an early menopause
- a person who has been taking steroids
IBD teams may measure blood levels of vitamin D and calcium if you are thought to be at risk of bone disease. Around 1 in 3 people with Crohn’s or Colitis have been found to be deficient in vitamin D.
Causes of Bone Loss in IBD
Experts point to several suspected causes for bone loss in IBD, including the following:
1. Corticosteroid therapy
These powerful anti-inflammatory medications can produce serious side effects, and bone loss is one of them. It is believed that 30-50% of people who take corticosteroids on a long-term basis develop Osteoporosis, and the effects are cumulative; with the impact on bone health depending largely on the dose and length of time that a person is on these medications. Corticosteroids impair the formation of new bone by:
- Decreasing the amount of calcium absorbed by the intestines from food
- Increasing the excretion of calcium in the urine
- Stimulating the production of cells that break down bone
- Decreasing the number of bone-forming cells
- Reducing the production of the hormone estrogen, which contributes to strong bones
2. Inflammation in active disease
People with IBD have elevated concentrations of specialized proteins, called cytokines, which increase the body’s inflammatory response. These chemicals may disrupt normal bone metabolism – the pace at which old bone is removed and new bone is formed. Individuals with more active forms of Crohn’s may be at increased risk of developing osteoporosis because their cytokine activity is greater. This connection also might explain why people with Ulcerative Colitis suffer less bone loss than those with Crohn’s disease. Although the two diseases have many similarities, they differ when it comes to cytokine balance.
3. Reduced absorption of nutrients
The nutrients important to bone formation, especially calcium and vitamin D, are absorbed in the small intestine. If you have extensive Crohn’s Disease that affects the small bowel, or have had parts of your small intestine removed, you may be at additional risk.
4. Avoiding dairy foods
If you do not eat dairy products, perhaps because of lactose intolerance or abdominal pain, you are more likely to have a shortage of calcium in your diet. Low levels of calcium can slow down bone formation.
5. Lower levels of sex hormones
The combination of inflammatory cytokines and reduced absorption of nutrients can lower levels of sex hormones (estrogen and testosterone). These hormones are important in maintaining bone health.
Preventive Measures
- Reduce steroid use; under your doctor’s supervision.
- Use steroid-sparing drugs such as Azathioprine, 6-MP, Methotrexate, Infliximab, or use Budesonide – an alternative to Prednisone, Budesonide is a systemic corticosteroid with fewer side effects than traditional steroids.
- Take medications to enhance bone health, which include the once-a-week bisphosphonate drugs Risedronate and Alendronate, the only drugs approved for steroid-induced osteoporosis. Both drugs work in the same way to prevent bone resorption and increase bone mineral density (BMD)
People with IBD also can take the following self-care steps to help prevent bone loss:
- Restrict alcohol consumption.
- Stop smoking.
- Engage in regular physical activity.
- Eat a diet rich in calcium or take 1,500 mg of calcium daily. If you don’t get enough natural exposure to sunlight, then dietary sources of vitamin D are essential. These include fortified milk, fish oils, and liver. Alternatively, take 400 units daily of supplemental vitamin D.
My experience
Next time… we explore how EIM’s look as an individual aspect of IBD care.

Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
Further Reading:
Crohns Colitis Foundation – Bone Loss in IBD
NIH – What People with Inflammatory Bowel Disease need to Know about Osteoporosis
Crohn’s and Colitis UK – Bones and IBD
IBD Clinic – IBD and Bones – Maintaining Bone Health
Everyday Health – Five Strategies for Building Better Bones Despite IBD
Disclaimer: This information is based on my own research into this particular extra intestinal manifestation of IBD as well as some personal experience and should not be used as medical advice. The suggested investigations and prevelance are part of the IBD protocols set out by NICE; but do vary between individual NHS Trusts and specific hospitals. If you seek advice regarding the things you experience within your own disease, please contact your IBD team for medical advice.