
“Why do you need B12 injections?”
I frequently get asked about my need to have regular top-ups of B12, via injection with my GP practice.
As a result of my first IBD surgery back in 2016, I require B12 injections due to deficiency.
Before I get into my own situation – the hows and whys – let’s answer some common B12 related questions –
1. Why might people with IBD be deficient in B12?
Anemia is a term used for a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. There are many types of anemia.
Pernicious anemia is a condition in which the body can not produce enough healthy red blood cells because it does not have enough vitamin B12. This is more commonly known as ‘B12 deficiency’ or ‘folate deficiency anemia’. It is more common in people who already have autoimmune conditions such as Crohn’s disease and ulcerative colitis which are both types of inflammatory bowel disease (IBD) due to surgery.
It can also occur in people who have had surgery to remove the stomach or the end of the small intestine for other reasons, ie gastric bang surgery, cancer, or complications from other stomach and bowel conditions.
2. Where is vitamin B12 absorbed and what does it do?
B12 is absorbed at the end of the small intestine – the terminal ileum – and people with Crohn’s disease in this area may not be able to absorb B12 as well as they should. The diagram below shows where important nutrients are absorbed in the small bowel, and you can see B12 is one of the very last to enter the bloodstream.
NB: I am unsure of the source of this diagram, so if you know who it is, please let me know so I can reference and credit!
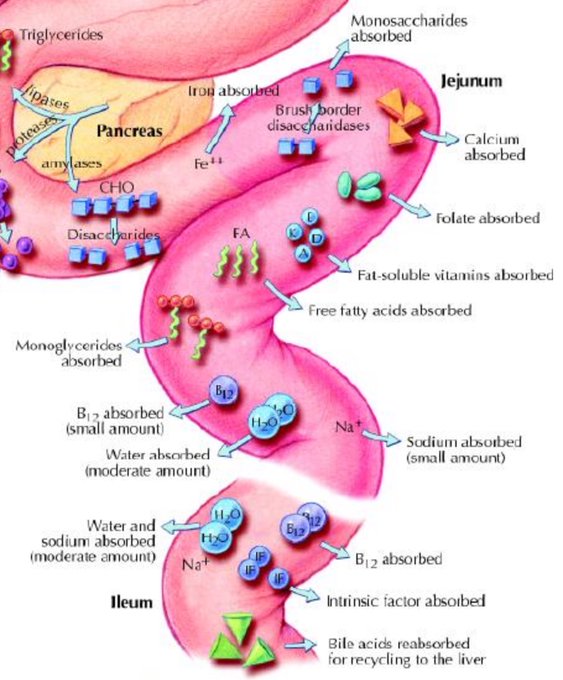
As you can see, any IBD surgery which removed the ileum – think limited small bowel resection, subtotal colectomy, right hemicolectomy, appendectomy – has a significant impact on B12 absorption.
B12 is very important in helping the body produce red blood cells – needed for oxygenation of the tissues in the body, specifically those in the bowel – and supporting the nervous system. B12 is naturally found in food – meat, fish, eggs, and dairy products – so it is easy to obtain a good level through diet. But if you suffer from a health condition, it might be more complex. However, most people can be easily treated with injections or tablets to replace the missing vitamins.
3. What the signs of a B12 deficiency?
Symptoms can include:
- Diarrhea or constipation
- Nausea
- Vomiting
- Fatigue, lack of energy, or lightheadedness when standing up or with exertion
- Loss of appetite
- Pale skin (mild jaundice)
- Shortness of breath, mostly during exercise
- Heartburn
- Swollen, red tongue or bleeding gums
If you have a low vitamin B12 level for a long time, you can have nervous system damage. These symptoms can include:
- Confusion
- Short-term memory loss
- Depression
- Loss of balance
- Numbness and tingling in the hands and feet
- Problems concentrating
- Irritability
- Hallucinations
- Delusions
- Optic nerve atrophy
4. What is the treatment for B12 deficiency?
Vitamin B12 deficiency anemia is usually treated with injections of vitamin B12.
There are 2 types of vitamin B12 injections:
- hydroxocobalamin
- cyanocobalamin
Hydroxocobalamin is usually the recommended option.
At first, you’ll have these injections every other day for 2 weeks or until your symptoms have started improving, usually given by our GP or nurse.
After this initial period, your treatment will change. Typically your level of B12 will be checked via a blood test and a treatment plan outlined for going forward.
If your vitamin B12 deficiency is not caused by a lack of vitamin B12 in your diet, you’ll usually need to have an injection of hydroxocobalamin every 2 to 3 months for the rest of your life.
If you have had neurological symptoms that affect your nervous system, such as numbness or tingling in your hands and feet, caused by a vitamin B12 deficiency, you’ll be referred to a haematologist and may need to have injections every 2 months. Your haematologist will advise on how long you need to keep taking the injections.
For injections of vitamin B12 given in the UK, hydroxocobalamin is preferred to an alternative called cyanocobalamin. This is because hydroxocobalamin stays in the body for longer. The reasoning behind this is because Cyanocobalamin would need to be given once a month, whereas hydroxocobalamin can be given every 3 months. Cyanocobalamin injections are not routinely available on the NHS as hydroxocobalamin is the preferred treatment.
For most people who have had a vitamin B12 or folate deficiency, they will not need further monitoring unless their symptoms return or their treatment is ineffective. But if your GP feels it’s necessary, you may have to return for an annual blood test to see whether your condition has returned or if a treatment change is required.
My B12 deficiency
My deficiency stems from my right hemicolectomy in 2016. But I didn’t have regular B12 injections until mid-2017 when I was seeking advice on some symptoms I was experiencing – fatigue, shortness of breath, confusion, and short-term memory loss. After some blood tests, we discovered my B12 levels were quite low, so injections began being a regular and routine part of my medical appointments. A little before a year of being on injections, we readjusted it from 12 weekly to 10 weekly which keeps my symptoms at bay better without much negative impact on my daily life.
Injections are one of the few things my GP practice allowed during the pandemic and lockdown to take place as normal. While a missed dose can be rectified, a prolonged gap between injections can make symptoms more frequent and last longer. Below are the teeny tiny vials of hydroxocobalamin, in which the vial top needs to be snapped off – so glad my nurses do this for me in a practice setting – before getting the liquid into a needled syringe. It needs to be given into the muscle and given very slowly, so it does sting and pinches a little. But the effectiveness of it far outways the pain of an injection. And you do kind of get used to it after a while.
I can usually tell when my B12 is low when my memory gets very fuzzy and I find it hard to form coherent sentences. This happens about 2 weeks before my injection is due, so it’s a good reminder check for getting my next appointment booked in. I can not have my injections early – before X date – but can have them a couple of days later – ie if it falls on a weekend or bank holiday.
I can not do these injections at home. They must be overseen by a health care professional and monitored by my own GP. Only they can reauthorise my prescription for them too.
Until next time,

Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
If you enjoyed this post check out A Practical Guide to Fatigue and “Are supplements helpful in IBD?”
Further Reading / Resources:
IBD Relief – Vitamin and mineral deficiencies in Inflammatory Bowel Disease (IBD)
NHS – Vitamin B12 or folate deficiency anemia – treatment
Nutrients MDPI 2017 – Associations between Folate and Vitamin B12 Levels and Inflammatory Bowel Disease: A Meta-Analysis – Yun Pan, et al
Oxford Press, June 2014 – Vitamin B12 deficiency in inflammatory bowel disease: prevalence, risk factors, evaluation and management – Robert Battat et al



1 Comments
"What does fatigue feel like?" • Young Crohns
23/02/2022 at 15:17
[…] If you enjoyed this post check out A Practical Guide to Fatigue and “Why do you need B12 injections?” […]