“Is mental health overlooked in IBD?”
How often when you get asked “how are you?” do you answer with regards to your mental or emotional health?
I get it, it is tough to really answer with a honest one. Especially when you’ve come to see a doctor about a physical problem.
But what happens when you’re physical problem is overshadowed by your emotions? Such as a chronic illness? How do you ‘separate’ the emotional from the physical?
In some ways, you can’t. It can be a very emotional thing dealing with something chronic – pain, discomfort, nausea, aches and tiredness. I find it very hard to separate my emotions from my physical pain at times. And in those times, we often get branded as ‘faking it’ because who wouldn’t be upset if they were in pain? Well, those who go through daily pain, can shut down the emotional part really well. It is still there for us, it is still real.
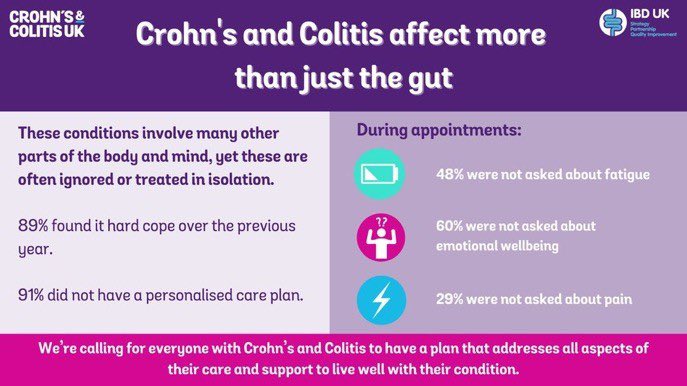
So is it any surprise that the below extract from IBD UK and Crohns and Colitis UK study is true?:
“48% were not asked about fatigue.
60% were not asked about emotional wellbeing.
29% were not asked about pain.”
These statistics make me sad. And then mad. But overall, it makes sense, sadly. Is there any priority for these sorts of questions in a 10, 15, 20 minutes conversation with a specialist when they are in so much demand? When appointments are being cancelled, postponed or even just not with the right person?
You can read full article here.
I get it, I do. I am a patient myself but also an advocate for helping the system be better and for patients to be heard more.
So many aspects of having a chronic illness can lead you to having issues with mental health. Low self esteem, anxiety, depression, PTSD, low confidence, body image and probably a whole host more. Do these come directly from having IBD? Is it medication? Is it surgery? Or is it all of it? Is having a chronic, life long condition, a hard and testing slog? Yes, yes and YES.
So, is mental health overlooked in IBD?
Heck yes.
Let’s not bang on about all the mistakes, all the negative experiences – even though, they add to the tapestry of the patient perspective and are not to be devalued or neglected in any way – but let’s focus on how we can make things better. How do we get mental health added into the conversation?
It won’t be a simple answer. Nor will it be straightforward or easy. But, it is necessary. And that makes it worth fighting hard for.
Step One: clinicians take some time in each appointment with a patient to gather some information about how they feel. Sometimes being asked or prompted can bring out an answer that might not have been saying previously. Being asked can also be the turning point in a new direction of care. If patients are, for example, experiencing no physical symptoms, could they be experiencing emotional issues? Could they do with some additional support? IBD is a complex fellow, and it is tough to manage and go through alone.
Step Two: access to appropriate support/care for mental health. If there are flags raised from consultations with patients, they need to be looked after. This step is more tricky and where I see alot of conflict occurring and vast differences between hospital and NHS Trusts. Access to mental health care is difficult and the pandemic and Covid 19 pandemic has made it more inaccessible because it is overloaded. More funding here is critical. But so would be funding IBD specific counsellors. We have made great strides with dietician care within IBD, I hope we can do the same for IBD mental health care.
Step Three: support becoming ‘normal’ and not the exception.
Thats the basic – very basic! – idea I’d thought about while research, drafting and writing this post.
For me, mental health access has been tough to get but worth it in the end. But waiting almost 6 months at times hasn’t been easy. Been ‘shoved’ onto antidepressants and then having them increased without any talk therapy or intervention has been dicey. I am fortunate to have not waited an incredibly long time, nor without support from friends and family for talking things through. And there is more accessibility through study and research within IBD and mental health where support is growing and evolving. All these things seem to be part of the system, and while it isn’t – and won’t ever be – perfect, it is something. We can keep fighting for better access, better support and more light being shed on this.

Until next time,

Do you have any questions or queries? Or just want to share your own experiences? You can leave me a reply here or leave comments via my social media accounts – on Twitter, find my blog page on Facebook and over on Instagram
If you enjoyed this post check out Being and Staying Positive and IBD & Mental Health
References:
Crohns and Colitis UK – Mental Wellbeing (pdf)
Cleaveland Clinic – Taking Care of your mental Health is a Key Piece of the IBD Puzzle
Healthline – UC & Mental Health
Crohns Colitis Foundation of America – Mental Health
Healio – Patients with IBD without a doubt struggle with mental health