The road to Vedolizumab
I write this on the eve of my first Vedolizumab infusion. Yes, we’ve gotten here awfully quickly, haven’t we?
Let’s go back to six weeks ago at the end of my last Infliximab infusion..
“Having me fail biological treatment like Infliximab was a shock. Back in the Spring when this first happened, I was happy to take baby steps forward and try building myself up to stronger, more potentially harmful treatments by gradually changing my current plan – decrease the time between doses and add in Methotrexate – before we gave up. And that was sound advice after my blood work showed low drug retention and high antibodies. I wasn’t expecting that, nor was my GI. I follow his guidance, I trust his opinion; even when he says he doesn’t know what to do. So to be told today that really, in hindsight we shouldn’t have done that, and they won’t do that in the future in the same circumstances; was disappointing. But I’m okay with it.”
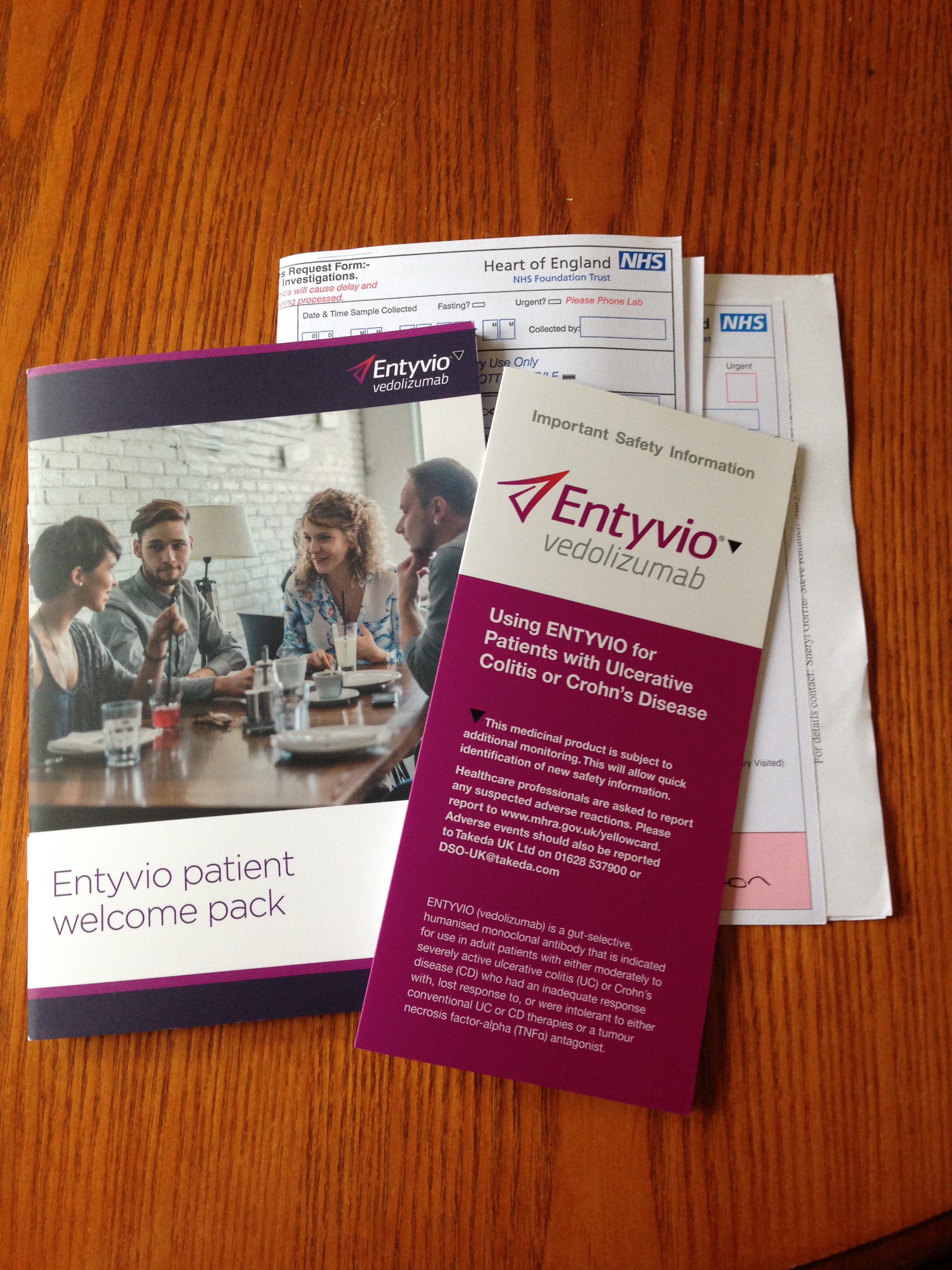
I have built up a really good relationship with my IBD nurse and she tells me straight how things will be. So she rattles off the usual side effects that could come with any biological treatment – headaches, coughs, colds, localised irritation, joint pain, nausea – then gets into the Vedolizumab specific ones and it hits me. I’m starting a new maintenance therapy and I’m exposing myself to a new drug. A drug targeted to reducing the white cells in my digestive system. This might work, it might not, but I’m going to be going back to square one again. That hits me hard, even thought I’ve almost always been on biological treatment since my diagnosis four years ago. It’s a shock. Some thing I’d not really consciously realised. I’m worried. What if this doesn’t work? It realistically has a 1 in 4 chance of working. I will be the second patient out of five selected thus far to receive this at the hospital. I’m going to be there every two weeks for six weeks before they let me have a maintenance schedule. It feels like a massive step back. Again.
This frustrates me as we go into see my consultant a hour later. At this point, I am considering maybe not having Vedolizumab and seeing if he has anything else up his experienced sleeves. After about two or three minutes, its clear he hasn’t got much left apart from trying to gauge my reaction – yet again, I might add – to experimental drugs and to a second opinion. The second opinion; I wanted regardless of being accepted onto the Vedolizumab program; so that is finalised and put into motion. So is the up-to-date MRI scan; that’s been requested too, finally.
It is clear that this is what is left for me to try. He has exhausted all options; he won’t try to increase MXT dose again, nor the Infliximab dose to double (10mg per kg instead of 5mg per kg) and without trailing experimental drugs, he needs more help with my case. Added to the fact I know I’ve lost more weight, have days when I can’t eat without pain and can feel – actually feel – blockages, its only a matter of time before my body reacts in a bad way. They have no choice but to get me onto a maintenance therapy, even if it is very unlikely to work.
So I leave feeling happier about things but not sure about what will really happen in the coming months.
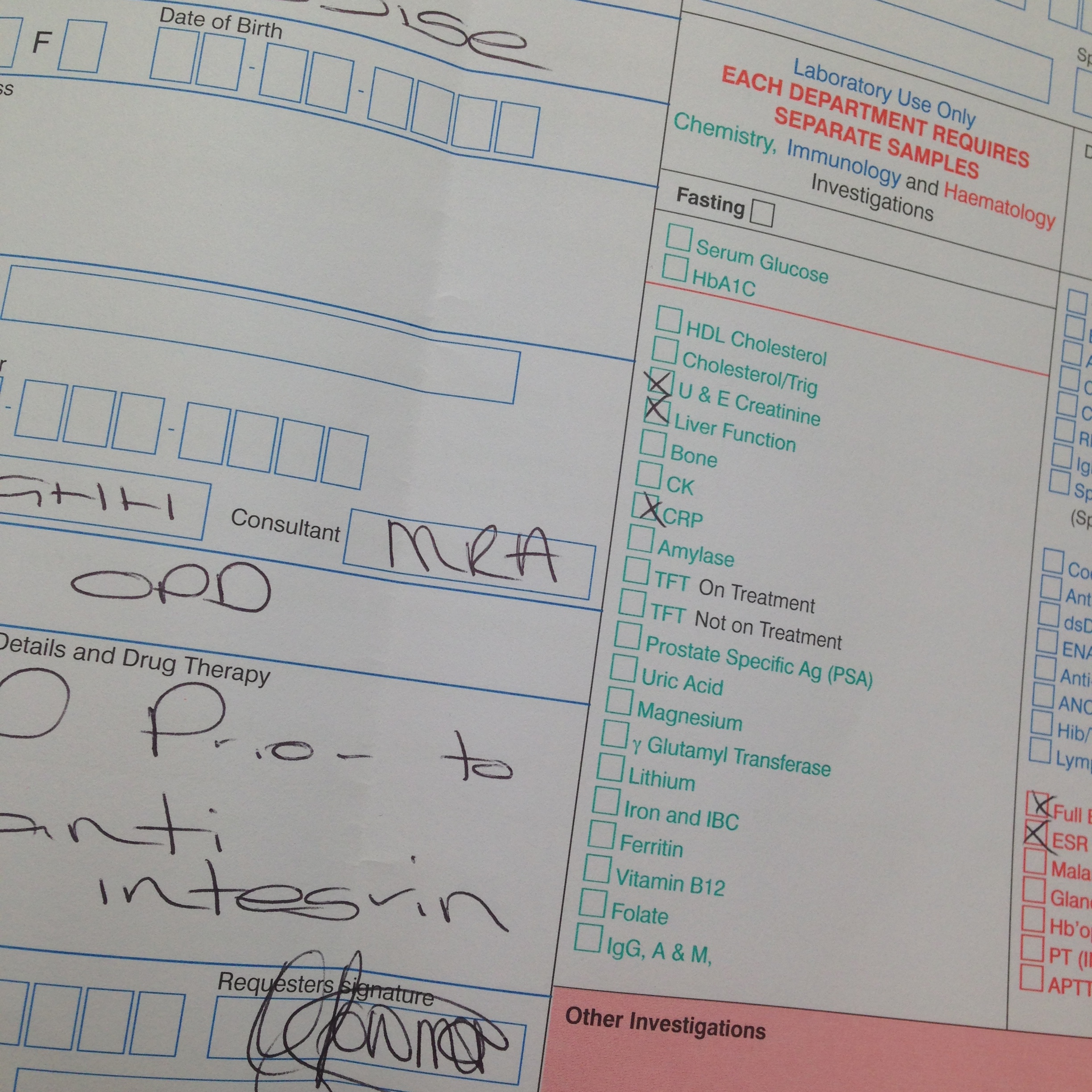
Fast forward a week; to Friday when I need to rush to the hospital to have the majority of my blood work (photos; both left and right) repeated – because it’s disappeared or not been done – so that I can actually attend the infusion clinic on Monday for my almost all day infusion.

It’s been a frightening and draining couple of weeks; organising to get the time of work to go for all my loading doses of Vedolizumab (two weekly intervals for six weeks; which just happen to fall at the end of my probationary period at my new job; typical!), then having to go in to have bloods taken, a chest x-ray done, waiting for results, the repeated blood work, let alone the nerves: anticipating tomorrow actually happening and getting started on a new chapter in this Crohn’s adventure.
I’m sure that it will be all fine but I wonder and worry alot about what this means, long-term.
If it means anything.
The best I can do is just hope for the best and deal with the worse, if and when it shows up.


2 Comments
Vedolizumab – Two Years On •
31/03/2021 at 10:09
[…] The Road To Vedolizumab [18.10.2015] […]
Vedolizumab Subcutaneous Injections •
03/11/2021 at 10:01
[…] you enjoyed this post check out The Road to Vedolizumab and Vedolizumab: Two Years […]