
I started this treatment in December 2013.
It works in the same way as Humira does, but has not be fully humanised. Infliximab must be delivered in hospital because of this reason; to keep patients under observations for side effects or reactions. Infliximab and Humira share the same side effects – lowered immunity, increased risk of infections and common illnesses.
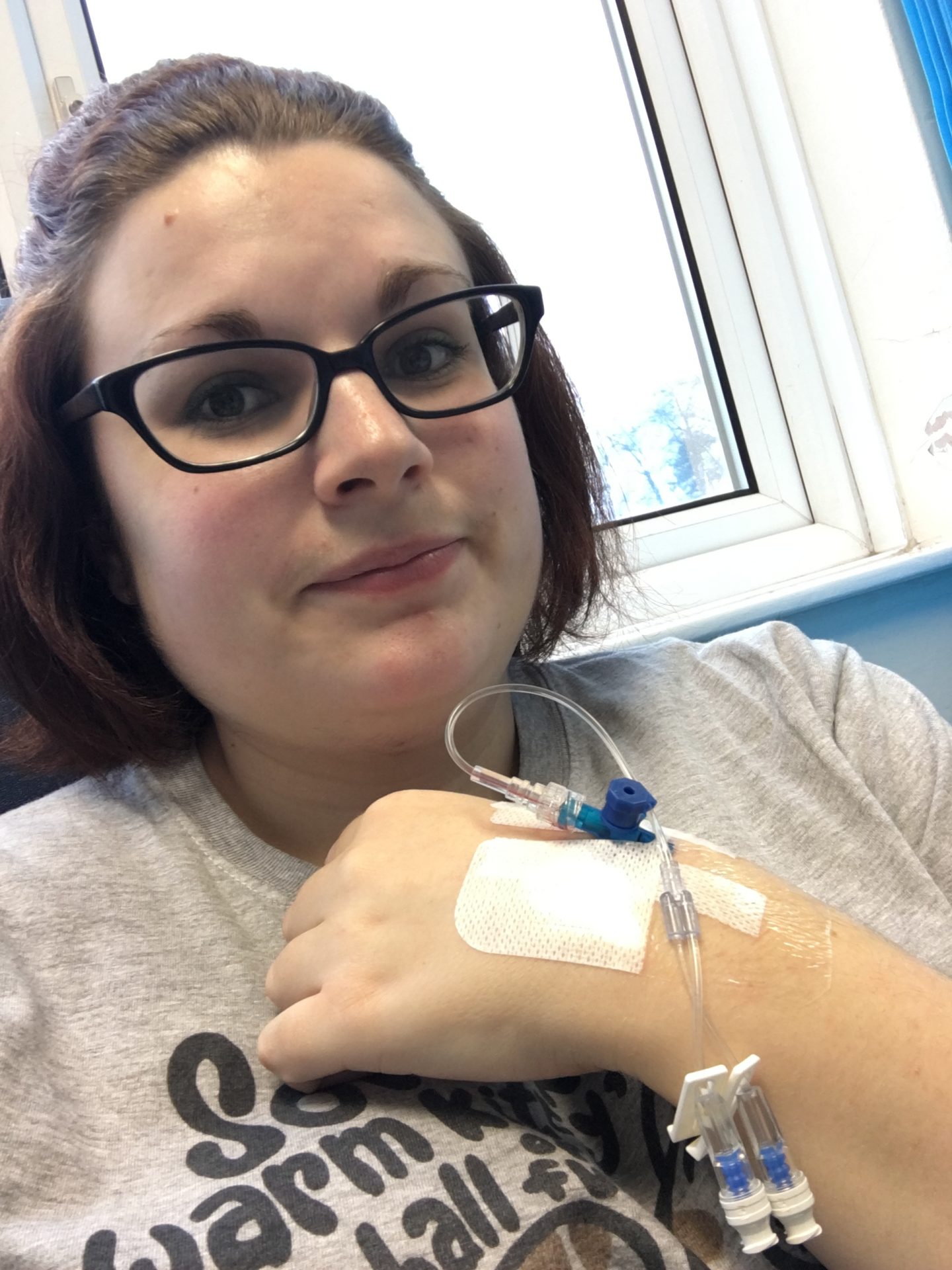
For my Inflixmab to take place, I had to have regular check up with my GI – between 8 weeks and 3 months – and pre-Inflixmab blood work. This was to check my CRP, LFTs and WBC to insure that I am healthy enough to take the medication. I also go through pre-sepsis checks – asked about my general health, if I have seen any other medical professionals in the prior two weeks and if I’ve receive any other medications – to avoid drug interactions and for my patient chart – or could be pregnant. I need to fulfil the criteria in order to receive my medication.
Seems contradictory; to be healthy enough to make sure I can take the medication, but my immunity is at its lowest following treatment meaning I was significantly more susceptible to colds and infections. This wasn’t a big issue in the first couple of months.

After a loading dose on Week One, I went back two weeks later for the second, and then returned four weeks after that to start the program properly. This period is critical; each patient is assessed to see how well their body has accepted the medication and if it is worth continuing. Luckily for me, I responded very well, despite not being ‘biologically native‘ – meaning I have a medical history of biological treatment (Humira) and might not have responded well to the same drug again.
My routine infusions took place at my local hospital every 8 weeks. The week before hand I’d need to go and have my blood taken, ready for my appointment with my infusion nurse. As the amount of infusions increases, the amount of time infusing and observing decreasing. I started with a two hour infusion and a two hour observation time for my first three infusions then down to a hour for each and finally after 6 infusions, down to just one hour infusion. This made it much easier to just spend a couple of hours there, instead of almost a whole day like I was in the beginning.
Reactions to biological treatment can happen at any point. My nurse makes a point of the “ten rule” – “10 minutes, 10 hours, 10 days” – to which a patient is likely to react. Whether or not this medication is continued is up to time, unfortunately. After just over a year on Infliximab – In early 2015 – I started to become symptomatic again. They decided to do specialist blood work – testing for antibodies and drug levels to see how well I was retaining the drug. It was soon found that I had extremely high antibodies and very low drug levels. This meant that my body was creating antibodies to the drug and was hardly retaining it in an eight weekly cycle.
First point of call was to add a secondary drug into my treatment plan to see if helped – Methotrexate. I had a loading dose of 10mg then moved up to 15mg and finally 20mg over a month. I had to take thrice-weekly folic acid to counteract the drugs side effects. It was hoped that this low-dose chemotherapy drug would help aid my drug levels and I would start to get more from the Infliximab. By the end of three months I had only made a slight improvement, so they increased my Infliximab to every six weeks. This was not good. I could only have three of these before they took the specialist blood work again and made a decision if Infliximab was working or failing. I knew I was coming close to having no treatment plans left to try to needed something to come along and help me out; at least until I was at a point where surgery was 100% necessary.
My experiences with Infliximab can be found here
More information about Infliximab can be found here.
More information about Methotrexate can be found here.
